Wellness
All Articles
Ticked Off: How to Recognize, Relieve and Resist Lyme Disease
Summertime is prime time for ticks, which are becoming more prevalent each year. A combination of changing land use and warmer winters has greatly expanded the ticks’ habitat and they’re…
Dementia and Alzheimer’s: Updates from a Leading Geriatrician
Senior Moments Or Something More? As Baby Boomers continue the inexorable journey deep into their senior years, preserving cognitive function understandably tops the list of worries. While Alzheimer’s Disease and…
Tips for Safe Summer Fun
Stay Safe with Sunscreen, Sunglasses and Plenty of Water The longer, sunshine filled days of summer are upon us and without a doubt, they are one of life’s unrivaled joys,…
Exercise Is Good Medicine
Get Up and Join the Movement As we emerge from the doldrums of winter hibernation and COVID-19-related inertia, it’s important to remember that exercise is good medicine and there’s no…
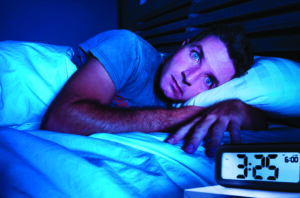
What’s Keeping You Up at Night?
Breaking the Cycle of Anxiety, Insomnia and Sleep Anxiety A good night’s sleep does more than refresh and revitalize. It’s essential to your health, so make it a priority to…
What Does BMI Really Tell Us?
Definitive Diagnostic Tool or Part of a Greater Health Matrix? It’s an easily understood calculation: Body Mass Index, popularly known as BMI, computes an individual’s measure of body fat as…
Pandemic Stress Likely Compounded by Seasonal Affective Disorder
Coping With Sad This Winter As we continue to weather the storm of COVID-19, seasonal affective disorder, or SAD, is once again on our radar. More subtle than an arctic…
A Novel Approach to Behavior Change
How to Replace Bad Habits with Healthy, Sustainable Behaviors For entrepreneur physician Kyra Bobinet, MD, the typical reasons behind a failed diet served as the impetus for developing a novel…
Staying Well in the New Year A Proactive Guide
In the spirit of starting 2022 with healthy intention, we’ve taken a page from the U.S. Preventive Services Task Force (USPSTF) latest recommendations, long considered the gold standard for clinical…
Color Your World with Every Hue of Fruit and Vegetable
Eating Your Fruits and Veggies May Help Reduce the Risk of Chronic Disease Fill your plate with a vibrant, colorful array of fruits and vegetables for a naturally delicious way…