Medical Tests
All Articles
What Does BMI Really Tell Us?
Definitive Diagnostic Tool or Part of a Greater Health Matrix? It’s an easily understood calculation: Body Mass Index, popularly known as BMI, computes an individual’s measure of body fat as…
COVID-19 VACCINE UPDATE 2.15.21
Update on Pre-Registration in state of Missouri Pre-registration Options Dear Patient, There are many options now where you can pre-register for a Covid-19 vaccine. These pre-registrations are non-committal and you…
Coronavirus Vaccine: Expert Says, ‘We Need Time to Get This Right’
Expert Calls for Slow & Steady Approach in Vaccine Development While the race to develop a coronavirus vaccine may seem as if it’s being run in slow motion, with most…
Colonoscopies Without Fear
Colonoscopies Without Fear Recognize Colorectal Cancer Awareness by learning more about this lifesaving screening. As… The post Colonoscopies Without Fear appeared first on Specialdocs Consultants.
Fighting the Colonoscopy Fear Factor
Colorectal Cancer awareness could save your life. As one of the country’s most preventable illnesses, with a readily available test that is both diagnostic and therapeutic, why does colorectal cancer…
Genetic Testing and Your Health
20,000 and You: Unlocking the Genetic Code In just the past few years, there has been a significant shift in the practical uses of genetic testing, which examines changes, or…
20,000 and You: Unlocking the Genetic Code
In just the past few years, there has been a significant shift in the practical uses of genetic testing, which examines changes, or variants, in your genes that may lead…
Unlocking the Genetic Code: Spotlighting Pharmacogenomics
This is the first in a series exploring some of the most promising advances inspired by the Human Genome project. From the burgeoning field of pharmacogenomics to consumer genetic testing…
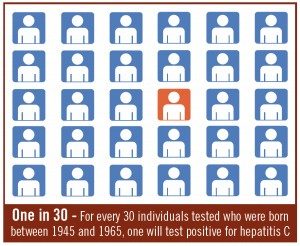
Hepatitis C Testing Recommended for All Baby Boomers
It’s called ‘the forgotten virus,’ but after a sustained advertising campaign and years of strong recommendations for testing by the Centers for Disease Control it’s almost certain that the liver-damaging…
Unlocking the Genetic Code: Spotlighting Pharmacogenomics
This is the first in a series exploring some of the most promising advances inspired by the Human Genome project. From the burgeoning field of pharmacogenomics to consumer genetic testing…